

Investigations Acute Cervical Lymphadenopathy (<2 weeks
Observation and reassurance without investigation is usually appropriate for the well-appearing child with cervical lymphadenopathy. May be associated with rash, joint pain, conjunctival changesĪpproach to differential diagnosis Management Persistent head and neck eczema may cause prominent posterior cervical LNs May be associated loss of appetite, weight loss, night sweats, easy bruising, hepatosplenomegaly, mediastinal mass Systemic features of fatigue or myalgiaĬonsider if prolonged, painless, firm lymphadenopathy. Non-suppurative generalised lymphadenopathy. Indolent, chronic unilateral cervical lymphadenopathy, violaceous hue, usually in children <5 yoīartonella henselae (cat scratch disease)Įnlarged nodes are usually tender and located in the axillary region Systemic symptoms of fever, malaise, weight loss May be associated with generalised lymphadenopathy and hepatosplenomegaly Many viruses will cause cervical lymphadenopathy lasting up to 6 weeks Chronic cervical lymphadenopathy (>6 weeks) - has a number of possible cause. Subacute cervical lymphadenopathy (2–6 weeks) – commonest cause viral infection. Kawasaki disease may present with unilateral tender cervical lymphadenopathy and associated features. Cervical lymphadenitis may rarely be associated with serious deep head and neck infections such a retropharyngeal abscess. A site of entry may be found (eg mouth or scalp). Common bacterial causes: Staphylococcus aureus, group B streptococcus (in neonates), group A streptococcus, and anaerobic infections (associated with dental disease). May be firm and tender with overlying erythema, limited neck range of motion. Associated with fever and neck swelling. Common, usually unilateral and in the anterior part of the neck. Small risk of developing into a secondary bacterial lymphadenitis. Usually resolves as other viral symptoms do. LNs may be tender to palpation and unilateral or bilateral. Very common, usually with history of a viral prodrome. Further examination should be guided by history and differential diagnosisĭifferential diagnosis Acute cervical lymphadenopathy Cervical lymphadenitis secondary to viral infection. Other focus of infection: scalp, face, ear, nose, throat or teeth. Features on palpation: eg soft, rubbery, firm, matted, fluctuant, discharging,. #POSTERIOR CERVICAL LYMPH NODES SKIN#
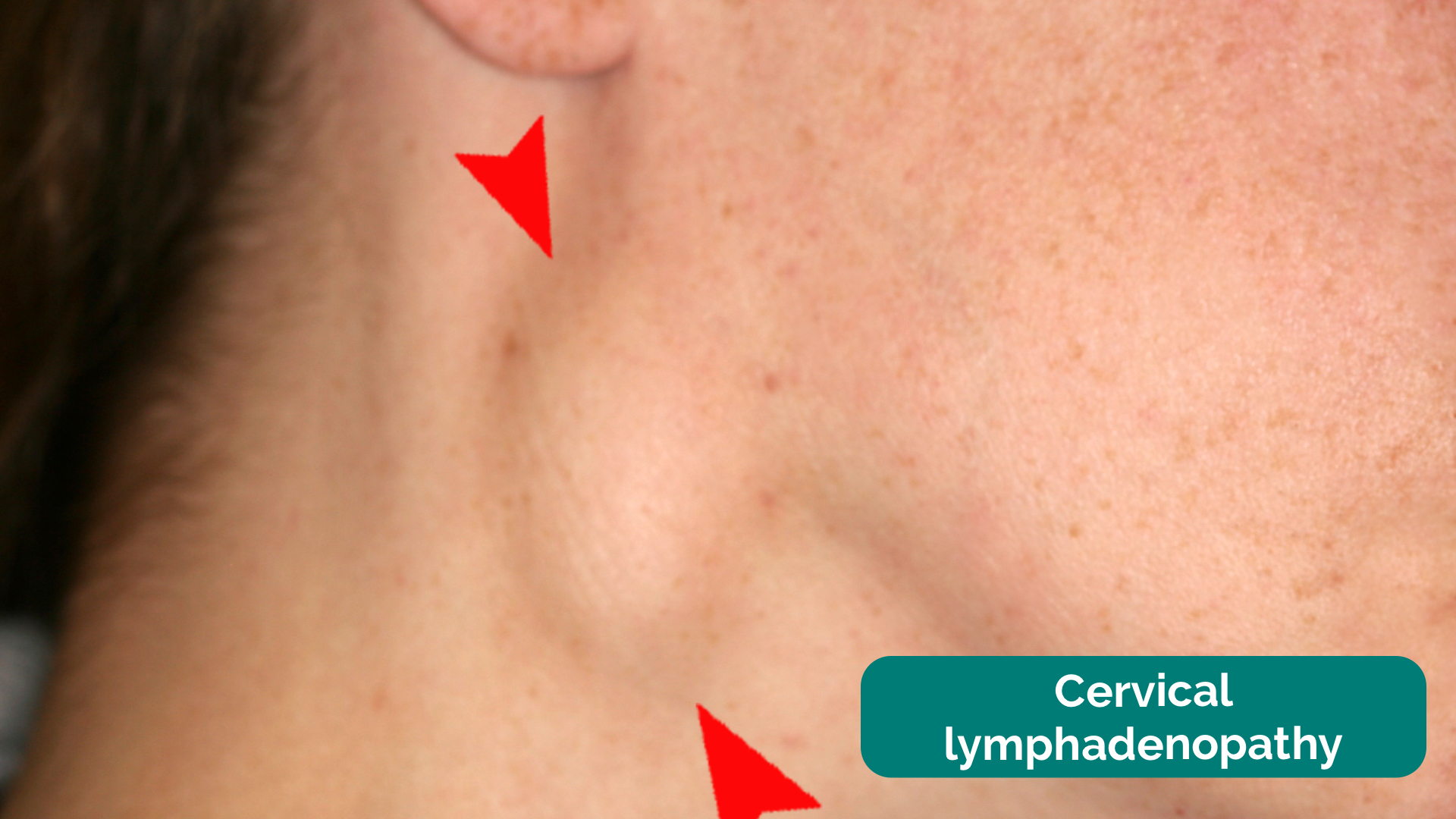
Characterise the lump: location, size, colour, warmth, mobility, tenderness, overlying skin changes.Immunisation status (diphtheria, measles, mumps, rubella).Overseas travel, including possible exposure to tuberculosis.Features of deep tissue head and neck infection (eg trismus, muffled voice).Growth over time, colour, pain, and overlying skin changes.Acute bacterial lymphadenitis is characterised by enlarged nodes, which are tender, usually unilateral and may be fluctuant.These enlarged "reactive" nodes may persist for weeks to months Viral upper respiratory tract infection is the most common cause of cervical lymphadenopathy in children.Most cases are benign and self-limited, however, the differential diagnosis is broad.Cervical lymphadenopathy is abnormal enlargement of lymph nodes (LNs) in the head and neck usually >1 cm.
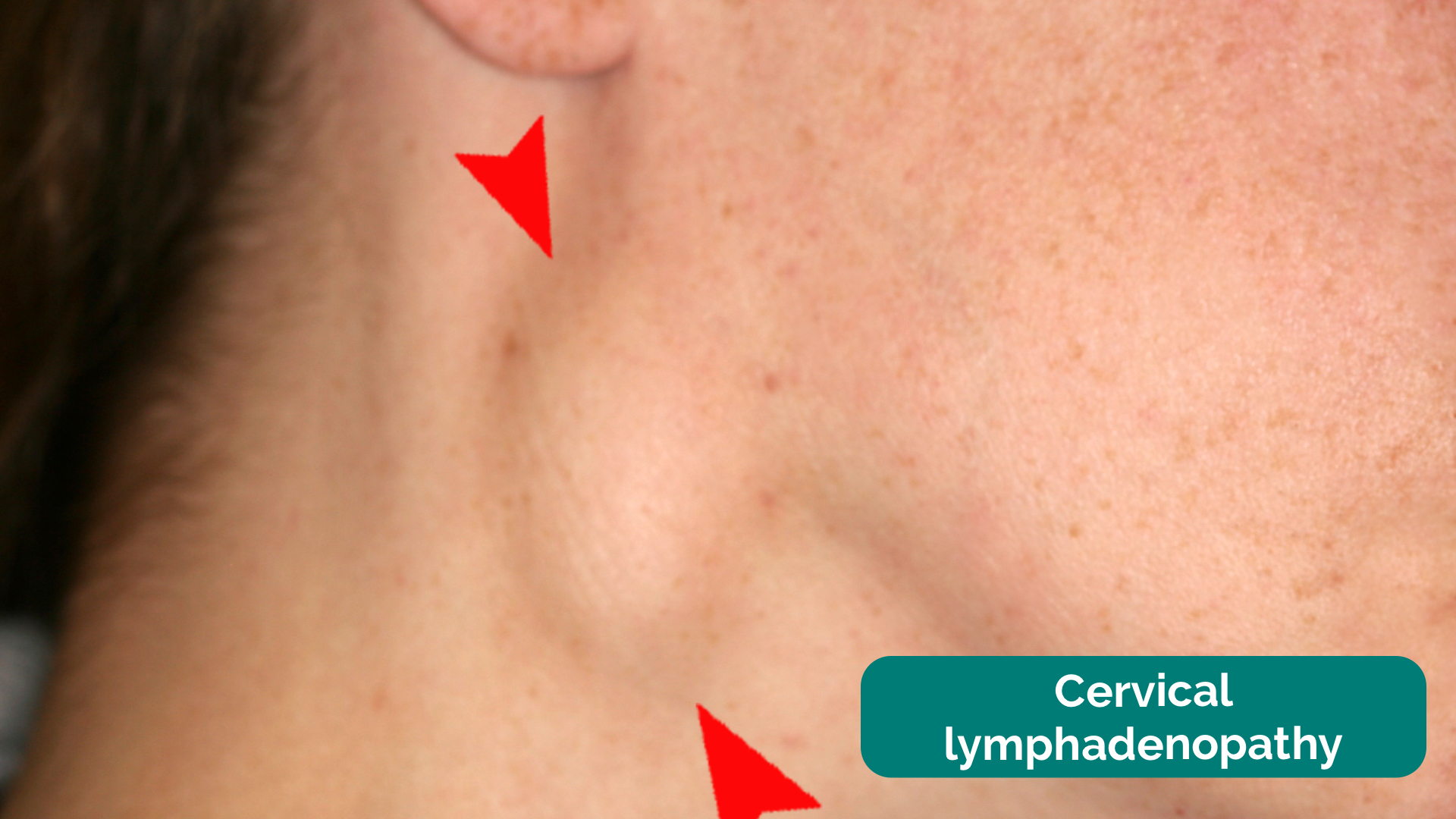
Cervical lymph nodes are often palpable in well children.Observation and reassurance without investigation is usually appropriate for the well appearing child with cervical lymphadenopathy.Cervical lymphadenopathy is common and may be found in more than one third of otherwise healthy children.





 0 kommentar(er)
0 kommentar(er)
